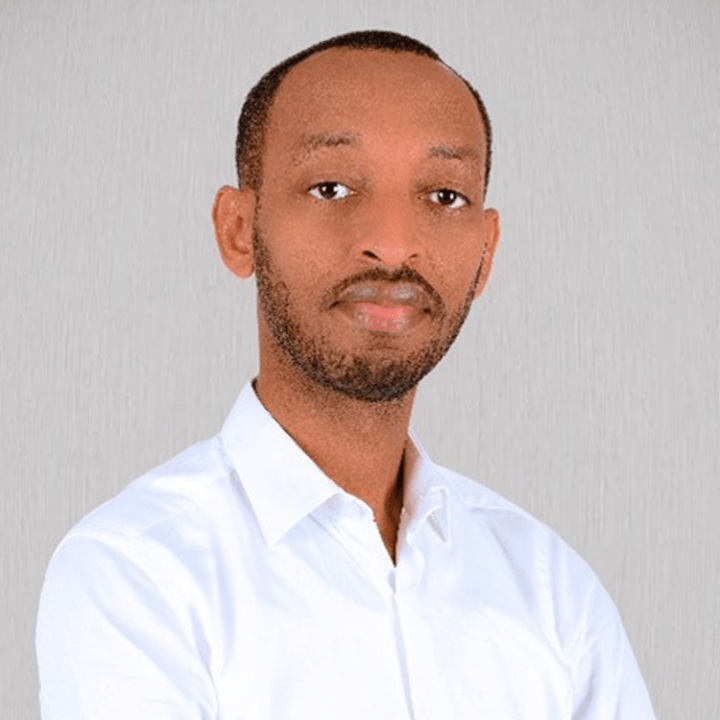
I spoke with Dr. Julien Nyombayire who is one of the leading vaccinologists in the region, and leads the Centre for Family Health Research (CFHR; also known as Projet San Francisco) in Kigali. Our discussion quickly reminded me that scientific discovery is rarely straightforward. He has spent the past 15 years working on HIV vaccine research – while the science itself is complicated, the story he tells is also one of persistence and dedication emphasising the importance of networks and capacity building to develop this important area of research.
Dr. Julien’s path into research began with what he calls a “very coincidental encounter” with the Centre’s former director, which led to him winning a scholarship that was being offered by the Center for young physicians. That introduced him to the world of research and clinical trials, which kicked off a 15-year long tenure at the CFHR. Step by step he built his career, and today, he leads a team coordinating major international studies, testing new vaccine candidates, and training a growing generation of researchers in Rwanda.
HIV Research as a Moving Target
Dr Julien shared that for over forty years, HIV has challenged scientists around the world. Unlike other viruses, where a vaccine can often be developed relatively quickly (as we recently saw during the COVID-19 pandemic), HIV constantly mutates, creating multiple strains even within the same individual. As he put it, “It’s a moving target.” Each promising research approach so far has brought more learning, yet a final solution remains elusive.
At CFHR, Dr. Julien and his colleagues are currently working on a fascinating new approach based on mRNA vaccine pathways. In late 2023, they helped lead a study to test the effectiveness of an mRNA-based HIV vaccine candidate (which demonstrated promising results based on prior research in the US) in Africa. The product was manufactured abroad, but everything else—the trial itself, the recruitment, the sample collection, and the laboratory analyses—took place locally. “This study… was the first in Africa and the first mRNA based HIV vaccine candidate, and it demonstrated that it worked a hundred percent. We can trigger those immune cells to later on develop these antibodies that we want,” he explained.
The trial was part of the ADVANCE network, a collaboration linking Rwanda with partners in Uganda, Kenya, South Africa, and other countries. The network pools expertise across the full research pipeline, from basic virology through to clinical testing. For Rwanda’s role, the trial was a way to showcase that African institutions can shape the direction of global vaccine research.
Still, the progress is not linear: Dr. Julien disclosed that results from animal models – which are typically used to test vaccines for safety and efficacy – do not always translate to humans, and promising lines of inquiry can (and very often do) reach dead ends. He takes this uncertainty as part of the work, and in fact his personal motivator: “Those question marks that remain in every step are also what trigger that interest to keep going.”
Clinical Research in Rwanda
Over the years, Rwanda has put structures in place that allow it to run clinical trials, meeting the same standards expected in high-income countries. Ethics and regulatory pathways are clear, and the country has invested in training and developing advanced laboratory infrastructure. Dr. Julien celebrates how this makes it possible to generate results in Kigali that can stand alongside those from Europe or North America.
Much of this strength rests on partnerships. Through ADVANCE and other networks, Rwandan researchers learn new experimental and laboratory techniques, while also training others from elsewhere on the continent. The mobility of skills—whether through senior scientists from the region visiting to mentor early-career staff or through nurses gaining experience across different trial sites—has helped Africa steadily expand its collective capacity. The sharing of research infrastructure between institutions further expands the continent’s repertoire for conducting end-to-end clinical trials.
Funding, however, remains the main constraint. With U.S. government funding (which was predominantly the main source of funding for HIV research) becoming less certain, African researchers are looking to Africa CDC and their national governments to support more of this work. The challenge is that, as Dr. Julien explains, “Vaccine research is very expensive, and it’s mainly because it’s a long process. You test one, you test five, ten products—only one works, and that’s the one you’ll be pursuing”. Research must also compete with other pressing priorities in health systems. Yet as Dr. Julien noted, these long-term research investments are critical. Without them, countries will struggle to be prepared for new and emerging health threats.
Looking Ahead: From HIV-Research to Genetics and NCDs
Although HIV-vaccinology remains central to his work, Dr. Julien recognises the priority for other research areas. He reflected on the reality that as healthcare treatment programs lengthen lives, and as populations age, non-communicable diseases (NCDs) such as cancer and cardiovascular disease are rising in prevalence and significance. This is the “double burden” of diseases—infectious disease alongside NCDs—and he believes research needs to adapt to this shift.
One area Dr. Julien sees as especially promising is genetics. “Genetics plays a role in almost all type of disease in NCDs as well as in communicable diseases because it has an impact on how we respond to these illnesses, how susceptible we are,” he explained. Understanding the interactions between genetics, the environment, and diseases could help shape gene therapies or preventive strategies in the long run. For Africa, this is still an underdeveloped field, but he sees it as a necessary investment for the coming decades.
A Word to Early-Career Researchers
When I asked him about advice for newcomers to research, Dr. Julien’s response was candid and encouraging. “You need to persevere, you need to love it so that you not get bored… because some of these are really repetitive processes. You repeat yourself many, many times.” He emphasized that research is rarely a straight path: sometimes a line of thinking must be abandoned entirely, not because it was wrong, but because the virus or disease outwitted the strategy.
What makes the work worth it, he told me, is knowing that every effort adds to our shared understanding. Although great strides have been made in HIV prevention and treatment with tools like Anti Retroviral Therapy (ART), “HIV is still a very real threat that still infects babies, still claims lives, and still resists easy solutions.” That reality continues to drive his commitment.
For Dr. Julien, the future of African research lies in persistence, strong networks, and steady investment in areas like genetics and NCDs. His own journey—beginning with a chance encounter, continuing one trial at a time—is a reminder that progress comes slowly, but it does come, as he said with a smile, “one step at a time.”




Leave a comment